NOTE: I am not a professional and this article does not constitute medical advice.
Always consult a doctor if you are seeking treatment for a condition such as Obstructive Sleep Apnea.
I’ll admit, it’s a bold claim: Tape your mouth shut, and you’ll be less likely to die. In this post, we’ll explore exactly how mouth taping, death, and health are related.
Have you ever woken up with an extremely dry mouth? Do you ever feel groggy and unrested, even if you get the recommended 7-9 hours of sleep? You might be breathing through your mouth at night – and mouth taping is a simple, effective, and cheap solution.
I had both of these symptoms – plus I snored like a champion. Once, while staying in a hostel, I was told by staff they could hear me all the way from the reception desk at night. Often, I woke myself up from snoring so loud.
In addition to being audible to everyone in a 100-meter radius, I noticed that I always woke up extremely tired, and with a parched mouth. This was the case even if I got lots of sleep the night before. No matter what, I would always feel like a zombie for at least a half hour after waking up.
I thought this was normal – I was just unlucky and not a “morning person”. Didn’t everybody need 30 minutes, a shower, and a cup of coffee to actually wake up?
Aside from the occasional embarrassment, I didn’t think much of my sleep problems. I didn’t have a significant other to endlessly torment, so the snoring wasn’t a big deal to me. My sleep habits were good enough, I figured, so I just kept trying to get enough sleep each night. I felt like crap, but carried on like nothing was wrong.
Seeking Sleep Solutions
The importance of getting a good night’s rest is unquestionable, with plenty of studies showing increases in all-cause mortality for those who fail to get a good night’s rest (or who sleep too much.)1 2 3
Uh-oh.
When I began to explore all areas of my health to try and improve it, sleep became one of the first things I focussed in on. Quickly, I dove headfirst into the world of sleep optimization and aids, looking into how to reduce snoring and improve sleep quality.
To name but a few things I tried:
-I cut down on caffeine (I’m back up to 6 cups a day…) and tried sedatives (RC Clonazolam to be specific)
-In an effort to exhaust myself into a deep sleep, I exercised vigorously an hour before bed.
-I reduced blue light before bed with F.lux and ‘night mode’ in iOS.
-And finally, I tried a myriad of products and solutions marketed at snorers: chin straps, specially designed pillows, sleeping on my side, and mouth taping.
In order to test out and compare these remedies by myself, I downloaded an app called SnoreLab. This allowed me to objectively record and track my snoring each night – and see whether a given product actually helped.
The chin strap and sleeping pills were the worst – they actually made my snoring even louder. Sedatives are known to worsen snoring: depressants such as alcohol or benzodiazepines relax the throat muscles and can make sleep apnea worse.4 However, I was disappointed the chin strap was so ineffective. My guess is that it exerted too much pressure on my jaw, and shifted my palate in a way that worsened my snoring.
I did find side-sleeping to be helpful, but only slightly. The problem was that I shifted a lot while I slept, and eventually ended up on my back anyways. For the purposes of staying temporarily quiet for your partner’s or roommate’s sake, though, it would be a good idea to incorporate side-sleeping.
Specialty pillows, mouth guards and other gadgets were simply uncomfortable or didn’t stay in place.
What stuck was mouth taping (pardon the pun).
Why Mouth Breathing is Bad
Why would you want to put tape on your mouth in the first place?
Ultimately, our noses are designed for breathing, and our mouths are for eating. Mammals all across the animal kingdom breathe through their noses by default, and humans are no different.5 However, our body is great at adaptation and survival. This means that if there is a nasal blockage preventing breath from being drawn from the nose, we can easily switch to breathing through our mouths – but this comes at a cost.
Poor Sleep, Concentration, and Health
Breathing plays a major role in regulating our sleep and the quality of the rest we get each night. Sleep apnea and other issues can arise when we no longer breathe through our noses.6 The effect is profound: one study found that “subjects with the nose obstructed awoke more often, had a greater number of changes in sleep stage, had a prolongation of rapid-eye-movement (REM) latency, and spent a greater amount of time in stage I non-REM sleep (light sleep).”7
“Mouth-breather” is a common pejorative for someone stupid – and there’s a reason for it. Mouth-breathers are more likely to have learning difficulties than nasal breathers,8 show deficits in memory recall, and score lower on Full Scale IQ, Performance IQ, and math achievement tests.9 Prevalence of mouth breathing has also been found to be strongly correlated with hyperactivity and ADHD.10,11 The evidence for poor breathing habits causing cognitive impairment is overwhelming.12
Mouth breathing and sleep-disordered breathing also cause poor oxygen concentration in the bloodstream and arteries.13,14 Sleep apnea leads to high blood pressure15 and hypertension,16 heart problems, and more. Another study found that introducing nasal obstruction in rats caused lasting physiological changes such as smaller lungs, and a 1000% spike in stress hormone release.17
When we mouth-breathe during sleep, we wake up feeling unrested, which affects our energy and ability to focus throughout the day. Our performance at work or school suffers.18 We become prone to aggressive outbursts, irritability, anxiety and depression.19
The consequences of mouth breathing are severe and wide-ranging – so let’s avoid doing that for 7-9 hours a day, shall we?
Facial Deformities
Most of the adverse physical effects of mouth breathing are of critical importance during childhood – when the structures of the jaw and mouth are still developing. There is a significant amount of research that shows the detrimental musculoskeletal effects of mouth breathing during growth. Perhaps the most striking examples are shown in this journal article, titled “Mouth breathing: Adverse effects on facial growth, health, academics, and behavior“.
It may be uncomfortable for some to hear, but the fact is that there are cross-cultural societal standards for what is considered attractive.20 These tend to be facial symmetry, and features such as high cheekbones, strong jawlines, straight noses, and nice teeth. Children that mouth breathe develop facial features that are the complete opposite: long soft faces, dark circles under their eyes,21 narrow nostrils with crooked or sunken noses, crowded teeth, and jaw problems (malocclusions) such as overbite.22
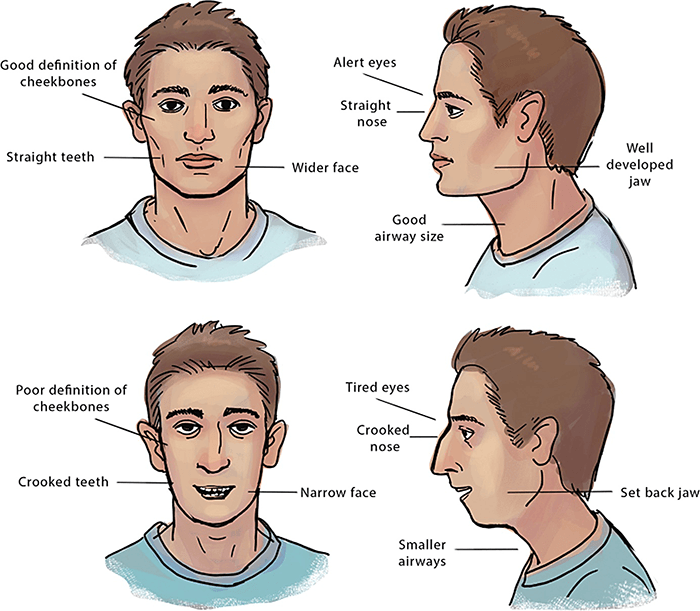
If you are at all concerned about the developmental health and well-being of your child, pay close attention to whether they breathe through their nose. It could mean the difference between braces and straight teeth.
Take, for example, this case of two sisters:
“Kelly was seven years old and Samantha was eight-and-a-half years old. Both sisters displayed habitual mouth breathing and were developing associated facial growth patterns. They attended Dr. Mew, who taught them to breathe through their noses and to swallow correctly.
Kelly took on all that Dr. Mew told her, but her older sister Samantha was more complacent. She did not keep her mouth closed while breathing.”
Both girls returned a few years later. Follow-up photographs are shown below.

Kelly is to the left and Samantha is to the right. Look at the startling difference in facial structure.
Don’t be like Samantha. Breathe through your nose.
Oral Hygiene
It turns out that mouth breathing is one of the worst things you can do for oral hygiene – and mouth taping easily prevents this. As discussed above, mouth breathing can lead to periodontal problems for children, but adults should take care to avoid this habit as well.
Mouth breathing has been shown to acidify the mouth,23 which is but one factor that leads to enamel erosion and cavities. Breathing through the mouth for 8 hours will also inevitably dry out your mouth, which can lead to halitosis24 and xerostomia. Your oral microbiome changes due to the lack of saliva, and harmful bacteria begin to proliferate.25
That something as simple as mouth breathing can lead to serious health consequences is surprising, but easily preventable.
Benefits of Mouth Taping
By now it should be clear we want to avoid breathing through the mouth whenever possible. During the day, you can simply make a concerted effort to be mindful of how you’re breathing and always breathe through the nose. But what about at night?
Well, it’s pretty obvious: if you tape your mouth shut, you will be forced to breathe through your nose. I know, shocking, right?
Using mouth tape during sleep is particularly important because we have no conscious control over our breathing during the night. The subconscious autonomous nervous system takes control, while our conscious minds wander off into the netherworld of dreams and rest. This means you may be inadvertently breathing through your mouth without even knowing it. A telltale sign is waking up with a dry mouth or fatigue.
Mouth taping will eliminate the possibility of mouth breathing at night, restore your respiratory function to its intended state, and bring with it a host of research-backed benefits.
Increased Nitric Oxide Levels
The sinuses and upper airway are responsible for producing almost all of the body’s nitric oxide.26 Scientists have only recently begun to investigate its role in biological processes, but so far we know nitric oxide is an important signalling compound and potent vasodilator. It promotes muscular relaxation and reduces inflammation,27 regulates oxygen absorption,28 and protects against cardiovascular disease.29 By breathing through the nose, you increase your intake of nitric oxide, and this in turn can increase the oxygen levels in your blood by up to 18%.30
Improved Rest and Relaxation
Breathing through your nose can lower your blood pressure,31 especially during exercise.32 The physiological relaxation-promoting effects of nasal breathing are particularly pronounced in yogic breathing exercises such as single-nostril breathing – studies found improvements in memory recall,33 parasympathetic tone,34 and changes in cardiovascular health35 among participants.
Reduction in Snore Volume
Lastly, many people find mouth taping significantly reduces their snoring or even eliminates it altogether. Studies show there is a correlation36 between mouth-breathing and sleep apnea, and encouraging nasal breathing may help reverse this.
Now, this is not something I can personally vouch for. However, I have not once woken up in the middle of the night since starting mouth taping. The snoring is still there for me, but with fewer massive gasps for air.
The overall benefits of mouth taping? Improved cardiovascular health, better sleep, mood, energy, and all-around performance.
What if my Nose is Congested?
If you suffer from allergies or asthma, this presents a challenge for always breathing through your nose – I would avoid jumping straight into mouth taping in this case. Your priority should be clearing out your nose and sinuses so you can actually breathe in the first place.
Thankfully there is an easy exercise that many have found helpful in decongesting their nasal passages naturally. The relief may be temporary, but you should notice an instant improvement. The good news is that with time, continuous nose breathing will naturally decongest the nose as the body adapts. It goes something like this:
- Take a small gentle breath in through your nose, and a gentle breath out through your nose, clearing out your lungs of air.
- Hold your breath while pinching your nose, to ensure air does not enter your lungs.
- Nod your head up and down, holding your breath for as long as possible.
- Release your nose to breathe through your nose again.
- Wait for about 30 seconds to a minute, and then repeat the exercise.
This exercise has been popularized by Patrick McKeown, author of “Close Your Mouth“. The book discusses using the Buteyko Method to relieve asthma, nasal congestion and snoring. The Buteyko Method is a series of breathing techniques that focus on nasal-breathing, breath-holding and relaxation.
If you want to look further into how our breath affects our health, I highly recommend his TEDx talk which can be viewed here:
Choosing the Right Mouth Tape
When I first started mouth taping, I just used whatever tape I found laying around for the first few days.
This ended up being outdoor carpet tape. No joke.
Honestly, probably not the best idea. Luckily the roll that I had in the garage was old and not-so-sticky, so I didn’t permanently seal my lips.
There are several tape options depending on how much you want to spend and your comfort level with peeling tape off your face each morning.
Budget Mouth Tape
3M surgical micropore tape is what I personally use. It’s strong enough to stay on all night and doesn’t hurt much when you take it off. A single roll lasts several months.
A box of 12 is super cheap:
Amazon
Gentle Mouth Tape
SomniFix strips are a step up in terms of comfort and design. They tout a specially-engineered adhesive that sticks without residue, and a small vent that allows a bit of mouth breathing.
Grab a pack here:
Amazon
Gel-Based Solution
If the thought of taping over your mouth makes you shudder, try SleepQ+, a gel-based product that lightly seals your lips while washing off easily in the morning.
They ship from Australia, so they’re the priciest option:
SleepQ+
How to Mouth Tape at Night
It’s pretty easy – pick up some tape, peel off a strip slightly longer than your lips, apply it to your mouth (pursing your lips slightly may help achieve a tight seal), and go to sleep. If using the micropore tape, folding a small edge over will help you take it off in the morning as you’ll have something to grab onto.
It may take a while to get used to – often people will unconsciously peel off the tape mid-sleep. I didn’t have this problem, but you can try applying the tape an hour or so before bed to get used to it.
My Mouth Taping Results
The first night I tried mouth taping (with the carpet tape, no less…), I woke up two hours ahead of my alarm, fully alert and rested. Instantly, I felt awake and energized, without coffee. This was shocking – all this clarity from simply taping my mouth shut. These days, I still snore relatively consistently. However, my quality of life has undoubtedly improved due to the increase in alertness, focus, and energy that nasal breathing brings.
I’m planning on doing a sleep study in a proper lab to assess whether I would benefit from a CPAP or other interventions to reduce snoring even further – but, for now, I’m noticing a big difference from just mouth taping and will continue for as long as necessary.
References:
- 1.Cappuccio F, D’Elia L, Strazzullo P, Miller M. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585-592. https://www.ncbi.nlm.nih.gov/pubmed/20469800.
- 2.Yin J, Jin X, Shan Z, et al. Relationship of Sleep Duration With All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J Am Heart Assoc. 2017;6(9). https://www.ncbi.nlm.nih.gov/pubmed/28889101.
- 3.Cai H, Shu X, Xiang Y, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015;38(4):529-536. https://www.ncbi.nlm.nih.gov/pubmed/25348122.
- 4.Guilleminault C. Benzodiazepines, breathing, and sleep. Am J Med. 1990;88(3A):25S-28S. https://www.ncbi.nlm.nih.gov/pubmed/1968716.
- 5.Trabalon M, Schaal B. It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr. 2012;2012:207605. https://www.ncbi.nlm.nih.gov/pubmed/22811731.
- 6.Lavie P. Rediscovering the importance of nasal breathing in sleep or, shut your mouth and save your sleep. J Laryngol Otol. 1987;101(6):558-563. https://www.ncbi.nlm.nih.gov/pubmed/3298509.
- 7.Olsen K, Kern E, Westbrook P. Sleep and breathing disturbance secondary to nasal obstruction. Otolaryngol Head Neck Surg. 1981;89(5):804-810. https://www.ncbi.nlm.nih.gov/pubmed/6799913.
- 8.Ribeiro G, Dos S, Santos A, Paranhos L, César C. Influence of the breathing pattern on the learning process: a systematic review of literature. Braz J Otorhinolaryngol. 2016;82(4):466-478. https://www.ncbi.nlm.nih.gov/pubmed/26832637.
- 9.Kaemingk K, Pasvogel A, Goodwin J, et al. Learning in children and sleep disordered breathing: findings of the Tucson Children’s Assessment of Sleep Apnea (tuCASA) prospective cohort study. J Int Neuropsychol Soc. 2003;9(7):1016-1026. https://www.ncbi.nlm.nih.gov/pubmed/14738283.
- 10.O’Brien LM, Mervis CB, Holbrook CR, et al. Neurobehavioral correlates of sleep-disordered breathing in children. J Sleep Res. June 2004:165-172. doi:10.1111/j.1365-2869.2004.00395.x
- 11.Huang Y-S, Chen N-H, Li H-Y, Wu Y-Y, Chao C-C, Guilleminault C. Sleep disorders in Taiwanese children with attention deficit/hyperactivity disorder. J Sleep Res. September 2004:269-277. doi:10.1111/j.1365-2869.2004.00408.x
- 12.Trosman I, Trosman S. Cognitive and Behavioral Consequences of Sleep Disordered Breathing in Children. Med Sci (Basel). 2017;5(4). https://www.ncbi.nlm.nih.gov/pubmed/29194375.
- 13.Swift A, Campbell I, McKown T. Oronasal obstruction, lung volumes, and arterial oxygenation. Lancet. 1988;1(8577):73-75. https://www.ncbi.nlm.nih.gov/pubmed/2891980.
- 14.Padzys G, Omouendze L. Temporary forced oral breathing affects neonates oxygen consumption, carbon dioxide elimination, diaphragm muscles structure and physiological parameters. Int J Pediatr Otorhinolaryngol. 2014;78(11):1807-1812. https://www.ncbi.nlm.nih.gov/pubmed/25193589.
- 15.Tanigawa T, Tachibana N, Yamagishi K, et al. Relationship between sleep-disordered breathing and blood pressure levels in community-based samples of Japanese men. Hypertens Res. 2004;27(7):479-484. https://www.ncbi.nlm.nih.gov/pubmed/15302984.
- 16.González-Pliego J, González-Marines D, Guzmán-Sánchez C, Odusola-Vázquez S. [Obstructive sleep apnea syndrome and hypertension. Evidence of their relationship]. Rev Med Inst Mex Seguro Soc. 2016;54(3):338-343. https://www.ncbi.nlm.nih.gov/pubmed/27100980.
- 17.Padzys G, Martrette J, Tankosic C, Thornton S, Trabalon M. Effects of short term forced oral breathing: physiological changes and structural adaptation of diaphragm and orofacial muscles in rats. Arch Oral Biol. 2011;56(12):1646-1654. https://www.ncbi.nlm.nih.gov/pubmed/21741618.
- 18.Urschitz M, Guenther A, Eggebrecht E, et al. Snoring, intermittent hypoxia and academic performance in primary school children. Am J Respir Crit Care Med. 2003;168(4):464-468. https://www.ncbi.nlm.nih.gov/pubmed/12773324.
- 19.Chugh D, Weaver T, Dinges D. Neurobehavioral consequences of arousals. Sleep. 1996;19(10 Suppl):S198-201. https://www.ncbi.nlm.nih.gov/pubmed/9085510.
- 20.Coetzee V, Greeff J, Stephen I, Perrett D. Cross-cultural agreement in facial attractiveness preferences: the role of ethnicity and gender. PLoS One. 2014;9(7):e99629. https://www.ncbi.nlm.nih.gov/pubmed/24988325.
- 21.De Menezes VA, Leal RB, Pessoa RS, Pontes RMES. Prevalence and factors related to mouth breathing in school children at the Santo Amaro project-Recife, 2005. Brazilian Journal of Otorhinolaryngology. May 2006:394-398. doi:10.1016/s1808-8694(15)30975-7
- 22.Grippaudo C, Paolantonio E, Antonini G, Saulle R, La T, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386-394. https://www.ncbi.nlm.nih.gov/pubmed/27958599.
- 23.Choi J, Waddell J, Lyons K, Kieser J. Intraoral pH and temperature during sleep with and without mouth breathing. J Oral Rehabil. 2016;43(5):356-363. https://www.ncbi.nlm.nih.gov/pubmed/26666708.
- 24.Motta L, Bachiega J, Guedes C, Laranja L, Bussadori S. Association between halitosis and mouth breathing in children. Clinics (Sao Paulo). 2011;66(6):939-942. https://www.ncbi.nlm.nih.gov/pubmed/21808855.
- 25.Mummolo S, Nota A, Caruso S, Quinzi V, Marchetti E, Marzo G. Salivary Markers and Microbial Flora in Mouth Breathing Late Adolescents. Biomed Res Int. 2018;2018:8687608. https://www.ncbi.nlm.nih.gov/pubmed/29693018.
- 26.Lundberg JON, Weitzberg E. Nasal nitric oxide in man. Thorax. October 1999:947-952. doi:10.1136/thx.54.10.947
- 27.Bian K, Doursout M, Murad F. Vascular system: role of nitric oxide in cardiovascular diseases. J Clin Hypertens (Greenwich). 2008;10(4):304-310. https://www.ncbi.nlm.nih.gov/pubmed/18401228.
- 28.Shibata M, Yamakoshi T, Yamakoshi K. Physiological role of nitric oxide in oxygen consumption by arteriolar wall. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:1389-1392. https://www.ncbi.nlm.nih.gov/pubmed/19162927.
- 29.Cooke J. The pivotal role of nitric oxide for vascular health. Can J Cardiol. 2004;20 Suppl B:7B-15B. https://www.ncbi.nlm.nih.gov/pubmed/15309199.
- 30.Lundberg J, Settergren G, Gelinder S, Lundberg J, Alving K, Weitzberg E. Inhalation of nasally derived nitric oxide modulates pulmonary function in humans. Acta Physiol Scand. 1996;158(4):343-347. https://www.ncbi.nlm.nih.gov/pubmed/8971255.
- 31.Stauss H, Persson P. Role of Nitric Oxide in Buffering Short-Term Blood Pressure Fluctuations. News Physiol Sci. 2000;15:229-233. https://www.ncbi.nlm.nih.gov/pubmed/11390916.
- 32.Petruson B, Bjurö T. The importance of nose-breathing for the systolic blood pressure rise during exercise. Acta Otolaryngol. 1990;109(5-6):461-466. https://www.ncbi.nlm.nih.gov/pubmed/2360451.
- 33.Garg R, Malhotra V, Tripathi Y, Agarawal R. Effect of Left, Right and Alternate Nostril Breathing on Verbal and Spatial Memory. J Clin Diagn Res. 2016;10(2):CC01-3. https://www.ncbi.nlm.nih.gov/pubmed/27042450.
- 34.Sinha A, Deepak D, Gusain V. Assessment of the effects of pranayama/alternate nostril breathing on the parasympathetic nervous system in young adults. J Clin Diagn Res. 2013;7(5):821-823. https://www.ncbi.nlm.nih.gov/pubmed/23814719.
- 35.Pal G, Agarwal A, Karthik S, Pal P, Nanda N. Slow yogic breathing through right and left nostril influences sympathovagal balance, heart rate variability, and cardiovascular risks in young adults. N Am J Med Sci. 2014;6(3):145-151. https://www.ncbi.nlm.nih.gov/pubmed/24741554.
- 36.Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnea. Acta Otolaryngol Suppl. 1996;523:228-230. https://www.ncbi.nlm.nih.gov/pubmed/9082790.




It’s been a few years since this article was written. Did you get a sleep study and do you still mouth tape or did you get a CPAP?
Hi Rob, great question! I did end up getting a sleep study in 2021, which showed an AHI of 40, indicating severe sleep apnea.
I now use a CPAP with nose-only headgear and it has helped a ton, and now only tape when travelling.